Published Oct 13, 2025 | 7:00 AM ⚊ Updated Oct 13, 2025 | 7:00 AM
In a normal pregnancy, fertilisation and the formation of the embryo take place in the fallopian tube, a process that depends on several factors aligning perfectly.
Synopsis: In recent years, fertility clinics in India have increasingly been relying on Artificial Intelligence tools to assist at nearly every stage of in vitro fertilisation, from selecting sperm for intracytoplasmic sperm injection to monitoring embryo development. Dr Radhika Potluri, Regional Medical Head and Fertility Specialist at Hyderabad-based Oasis Fertility, explains how these tools improve accuracy and reduce risks.
In a fertility clinic in Hyderabad, Dr Radhika Potluri watches as an embryologist peers through a microscope at a droplet containing dozens of sperm cells. The embryologist must select just one – the single cell that will be injected into a waiting egg during intracytoplasmic sperm injection (ICSI).
Traditionally, this process takes an hour or two as the embryologist manually assesses the shape, movement, and morphology of each sperm cell. These days, the process is much faster, thanks to neural network-based artificial intelligence (AI) tools.
“With AI-based grading systems, the same task can be completed much faster. The software rapidly screens and grades thousands of sperm, allowing us to choose the healthiest one for fertilisation,” explains Dr Potluri, Regional Medical Head and Fertility Specialist at Oasis Fertility, Hyderabad, to South First.
From predicting how patients respond to ovarian stimulation to selecting embryos most likely to result in healthy pregnancies, AI tools now assist at nearly every stage of the IVF process.
The technology promises to make fertility treatment safer, more efficient, and more successful – particularly important in a country where IVF remains expensive and many couples can afford only one or two attempts at parenthood.
In a normal pregnancy, fertilisation and the formation of the embryo take place in the fallopian tube, a process that depends on several factors aligning perfectly. IVF helps couples for whom this process does not occur naturally.
“[It] could be due to blocked or damaged fallopian tubes, poor sperm quality or low sperm count, or situations where the eggs are few in number or not being released properly. In such cases, we collect the eggs and sperm, allow them to fertilise in the lab, and then transfer the resulting embryo into the uterus,” Dr Potluri explains.
The process involves multiple stages where decisions determine success or failure.
Which medication dose will stimulate optimal egg production? Which sperm cell has the best chance of fertilising an egg? Which embryo will implant successfully? Which day offers the best window for transfer?
For decades, doctors made these decisions based on clinical experience and subjective observation. That began to change in 2022, when a team led by Dr Alejandro Chávez-Badiola in Mexico City pioneered one of the earliest applications of artificial intelligence in reproductive medicine.
In a paper published in Reproductive BioMedicine Online the same year, Chávez-Badiola’s team recorded ICSI procedures and analysed them using software called SiD v1.0. The programme tracked 383 individual sperm cells from 78 IVF cycles, calculating three parameters for every single sperm in the field of view.
It measured straight-line velocity—how fast each sperm travels in a direct path. It computed linearity—how much the sperm deviates from that path. And it quantified head movement pattern, a value that captures the oscillation and rotation of the sperm head as it swims.
What the researchers discovered changed how fertility specialists understand sperm selection. Sperm chosen by embryologists had significantly higher values for all three parameters.
Sperm with more linear trajectories and larger variations in head movement patterns fertilised eggs more successfully. When those fertilised eggs developed into blastocysts—the five-day-old embryos ready for transfer—they came from sperm with higher straight-line velocity.
“The motility characteristics of spermatozoa may be linked to the overall function and fertilisation potential,” the researchers wrote. The software ranked each sperm and assigned it a score. Sperm that achieved successful fertilisation had significantly higher scores. Sperm that produced blastocysts scored even higher.
“The possibility of carrying out real-time analyses of individual spermatozoa using an automatic tool such as SiD creates the opportunity to assist the embryologist in selecting the better spermatozoon for injection in an ICSI procedure,” the authors concluded.
Dr Radhika Potluri describes how these tools address one of fertility medicine’s most challenging scenarios.
“At present, the main areas where we use artificial intelligence in IVF are sperm selection and embryo selection,” Dr Potluri explains.
“There are now advanced AI tools that help us even in cases of azoospermia, where the sperm count is almost zero. In such situations, the AI can scan through thousands of cells to identify one or two viable sperm that might otherwise be missed.”
The software analyses motion patterns indistinguishable to human observers. The flagellum’s helicoid beat pattern, the sperm head’s oscillation, and the velocity of movement through a viscous medium all contain information about the cell’s capacity to initiate life.
“From all these factors, experimental and theoretical evidence strongly suggests that the flagellum’s helicoid beat pattern is essential,” Chávez-Badiola’s research team noted. The study showed that embryologists intuitively select sperm with these characteristics, but AI quantifies and accelerates that process.
The system works with existing microscopes found in most fertility laboratories. It requires no special chemical compounds, microfluidic devices, or custom equipment. The software identifies which objects in a sample are sperm, determines whether those sperm are in the focal plane near the injection needle, and ranks them in real time.
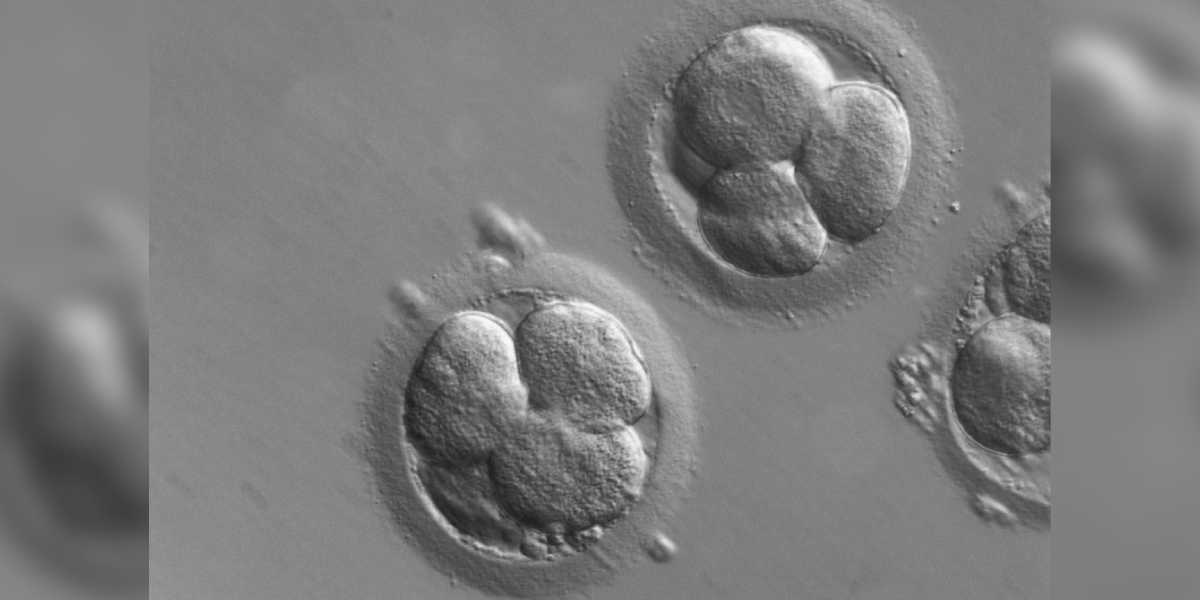
But sperm selection is only the beginning. The transformation continues after fertilisation, when a single cell begins dividing into two, then four, then eight, then sixteen. Eventually, it hollows out and reorganises into a blastocyst – a sphere of cells with a fluid-filled cavity and a compact inner mass that will become the foetus.
For decades, embryologists graded these embryos by observing them under a microscope once a day. They assessed the size and symmetry of cells, the compactness of the inner cell mass, and the texture of the outer layer. Grades were assigned in letters and numbers—AA, AB, BB, BC—based on subjective visual assessment and the embryologist’s experience.
“In earlier days, after performing ICSI, we had to wait until Day 5 to check the embryos under a microscope and grade them manually based on their appearance. But with AI-enabled time-lapse imaging, we can now monitor the embryo’s development continuously,” Dr Potluri explains.
“A camera fixed inside the incubator captures images of the embryo every few seconds during its five-day growth period. The AI then analyses these images to detect how the embryo is dividing and developing. It helps us identify the healthiest embryos and spot abnormalities early, improving both accuracy and success rates.”
Time-lapse systems generate thousands of images per embryo over five days. Patterns emerge in the timing of cell divisions, in morphology at specific developmental stages, and in subtle textures and gradients visible only through computational analysis.
It is too much data for humans to process efficiently – but ideal for artificial intelligence.
The use of AI in IVF begins even before the eggs are retrieved: during the ovarian stimulation phase, when patients receive daily hormone injections to produce multiple eggs in a single cycle.
“When a patient comes to us, we first evaluate how she might respond to ovarian stimulation – whether she is likely to be a poor responder, a hyper-responder, or somewhere in between,” Dr Radhika Potluri explains. “Traditionally, we make these decisions based on hormone levels, previous treatment history, and our clinical experience. But technology, especially AI, brings much more precision to this process.”
AI tools analyse hormonal profiles to predict patient response. They recommend precise medication doses, reducing the risks of over- or under-stimulation. They also identify conditions such as polycystic ovary syndrome (PCOS) or early ovarian ageing. Though not yet widely deployed in India, these systems are gradually being integrated into clinical practice.
“With AI, the process becomes more accurate and individualised. The system can recommend the exact stimulation dose a patient needs, reducing the risks of over- or under-stimulation. It can also help identify conditions like polycystic ovary syndrome or early ovarian ageing more effectively,” Dr Potluri said.
“During stimulation, we usually perform ultrasound scans every alternate day to monitor the ovarian response. In routine practice, these scans are done by different doctors on different days, which can sometimes lead to inter-observer variation – small differences in how follicle growth or ovarian size is measured.”
AI eliminates these inconsistencies by providing standardised measurements and analysing growth trends over time. This accuracy ensures that ovulation triggers and egg retrievals occur at the optimal moment – a factor crucial to IVF success.
“AI helps eliminate these inconsistencies by providing exact and standardised follicle measurements and by analysing growth trends over time. This accuracy ensures that we trigger ovulation and perform the egg retrieval at the correct moment,” Dr Potluri explains.
“With AI-guided monitoring and dose adjustment, we can significantly reduce the risk of ovarian hyperstimulation and other complications. It makes the process safer, more efficient, and ultimately more patient-friendly.”
The technology continues to evolve. Emerging systems measure endometrial thickness, determine the precise window of implantation when the uterus becomes most receptive, and monitor hormonal patterns to predict the ideal time for embryo transfer.
“Some of the recent studies suggest that AI can also help us obtain highly accurate imaging of the embryo, measure the endometrial thickness, and even determine the exact ‘window of implantation’ – that is, when the uterus is most receptive for embryo transfer,” Dr Radhika Potluri notes.
“It can also assist in monitoring hormonal patterns, such as progesterone levels during the luteal phase, and predict the ideal time to provide hormonal support. These technologies are still emerging, but the potential is very promising.”
The goal is synchronisation – matching the right embryo with the optimal moment for transfer, ensuring that the uterine environment offers maximum receptivity.
“In the future, AI could help us synchronise everything – selecting the right embryo, identifying the perfect moment for implantation, and ensuring the uterine environment is fully receptive. All of this can work together to significantly improve pregnancy rates,” Dr Potluri says.
The transformation also extends to how fertility specialists understand their own expertise. For decades, embryologists have trained by observing thousands of embryos, developing intuition about which ones are most likely to succeed. That intuition worked, but it remained locked within individuals – variable across practitioners, and difficult to standardise or systematically improve.
AI externalises that expertise. It converts visual patterns into numbers, intuition into algorithms, and experience into training data. The software learns from every embryo it analyses, improving as datasets expand. It makes the invisible visible, the intuitive explicit, and the subjective objective.
“Ultimately, this technology helps us improve pregnancy outcomes, reduce risks, and increase the overall success rate of IVF. It’s making the process not only faster but also safer and more precise for patients,” Dr Potluri says.

